| << Previous 1 - 2 Next >> |
March is Nation Kidney Month
by www.niddk.nih.gov/health-information/community-health-outreach/national-kidney-m | March 1, 2024
National Kidney Month 2021

March is National Kidney Month, a time when communities across the country raise awareness about kidney disease. This year’s focus is on taking charge of your health and the many factors that go into managing your kidney disease.
Chronic kidney disease (CKD) is a serious condition affecting 37 million people. Often overlooked until symptoms appear, CKD is progressive and can put you at risk for serious health complications including kidney failure. Adopting a healthy lifestyle can help you manage and slow progression of CKD and its complications.
Follow these healthy lifestyle tips to take charge of your kidney health.
- Meet regularly with your health care team. Staying connected with your doctor, whether in-person or using telehealth via phone or computer, can help you maintain your kidney health.
- Manage blood pressure and monitor blood glucose levels. Work with your health care team to develop a plan to meet your blood pressure goals and check your blood glucose level regularly if you have diabetes.
- Take medicine as prescribed and avoid NSAIDs like ibuprofen and naproxen. Your pharmacist and doctor need to know about all the medicines you take.
- Aim for a healthy weight. Create a healthy meal plan and consider working with your doctor to develop a weight-loss plan that works for you.
- Reduce stress and make physical activity part of your routine. Consider healthy stress-reducing activities and get at least 30 minutes or more of physical activity each day.
- Make time for sleep. Aim for 7 to 8 hours of sleep per night.
- Quit smoking. If you smoke, take steps to quit.
It may seem difficult, but small changes can go a long way to keeping your kidneys and you healthier for longer.
Prostate Awareness Month
by https://www.whitehouse.gov/live/ | September 1, 2023
A Proclamation on National Prostate Cancer Awareness Month, 2023
This year alone, more than 280,000 Americans will be diagnosed with prostate cancer. During National Prostate Cancer Awareness Month, we honor the lives ended too soon and all those we can still save by redoubling our efforts to end cancer as we know it.
When someone is diagnosed with prostate cancer, every second counts. But patients are too often left advocating for basic care while drowning in a flood of medical information. Even when treatment is available, some struggle to afford it or insurance may not cover it. And stark inequities exist: Black men are more than twice as likely to die from prostate cancer in this country than other men.
Our Nation must do more to change that. Last year, the First Lady and I reignited the Cancer Moonshot, setting an ambitious new goal to cut America’s cancer death rate by at least half over the next 25 years, turning more cancers from death sentences into treatable diseases and improving support for patients and families. I worked with the Congress to establish the Advanced Research Projects Agency for Health, securing $2.5 billion in bipartisan funding to develop breakthroughs in preventing, diagnosing, and treating cancer and other deadly diseases and pioneering partnerships to get those breakthroughs out to clinics and patients. We are making lifesaving cancer care more affordable for millions of Americans, expanding coverage through Medicaid and the Affordable Care Act, and helping many who had received relief during the pandemic to keep saving $800 a year on insurance premiums. The Inflation Reduction Act will soon cap total out-of-pocket prescription drug costs for seniors on Medicare at $2,000 a year — including for expensive cancer medicines — which could save some prostate cancer patients up to $6,000 a year.
We are also working to make sure prevention, detection, and treatment procedures are available to patients of all communities and backgrounds. The National Institutes of Health is continuing expansive research into environmental and genetic factors to better understand why prostate cancer disproportionately affects Black men. In response to our Cancer Moonshot, the Department of Veterans Affairs expanded its National Precision Oncology Program to better tailor treatments to individual veterans. And we know that screening matters: Experts recommend that men with a higher risk of cancer — based on race or ethnicity, family history, or other factors — discuss it with their doctors.
Everyone’s journey with cancer is different, but the First Lady and I know how hard it can be on the whole family. To all those caring for loved ones with prostate cancer and all those facing it themselves, we stand with you. My Administration is working around the clock on breakthroughs that can bring hope and more choices to the fight against this disease.
NOW, THEREFORE, I, JOSEPH R. BIDEN JR., President of the United States of America, by virtue of the authority vested in me by the Constitution and the laws of the United States, do hereby proclaim September 2023 as National Prostate Cancer Awareness Month. I encourage citizens, government agencies, private businesses, nonprofit organizations, and other interested groups to join in activities that will increase awareness of what Americans can do to prevent and cure prostate cancer.
IN WITNESS WHEREOF, I have hereunto set my hand this thirty-first day of August, in the year of our Lord two thousand twenty-three, and of the Independence of the United States of America the two hundred and forty-eighth.
JOSEPH R. BIDEN JR.
National Minority Mental Health Month
by https://afsp.org/story/the-role-of-the-church-in-improving-mental-wellness-in-th | July 1, 2022
The Role of the Church in Improving Mental Wellness in the African American Community
1 Feb 2021 — 4 min read
Jul. 23, 2019 - July is National Minority Mental Health Awareness Month, which was established in 2008 to bring awareness to the unique struggles that underrepresented groups in the United States face regarding mental illness. Clearly, mental health conditions do not discriminate based on race, color, or gender identity, yet we see stark differences in access to, and utilization of, treatment resources. Approximately 1 in 5 adults in the U.S. (46.6 million) experiences mental illness in a given year, regardless of their race.1 Fewer than half of adults in the U.S. with a mental health condition receive mental health services in a given year. African Americans however, utilize mental health services at about one-half the rate of Caucasian Americans.2 This begs the question: why?
We cannot rule out the impact of historical adversity, which has led to race-based exclusion from health, educational, social and economic resources. Many African Americans today still feel the socioeconomic impact of slavery, sharecropping, and Jim Crowism. Socioeconomic status is linked to mental health, in that people who are impoverished, homeless, or incarcerated are at higher risk for poor mental health. We also cannot rule out the impact of stigma associated with mental illness in the African American community. According to the Health and Human Services Office of Minority Health, African-Americans are 20% more likely to experience serious mental health problems than the general population, yet African Americans are less likely to initiate treatment and more likely to end treatment prematurely.
Literature suggests that African Americans are much more likely to rely on their faith as a coping mechanism for dealing with depression and anxiety than they are to utilize a mental health professional. One study found that 90.4% of African Americans reported use of religious coping in dealing with mental health issues.3 In other words, many African Americans, rather than seeking support in the form of a mental health professional, go to the church.
This is not surprising when one understands the traditional role of the African American Church. There has always been a connection to faith and the emotional well-being of African Americans. I can remember personally, sitting on the front pew of the church, the son of a pastor, watching in awe as my father recited spirited sermons from the pulpit as the congregation hung on every word. After church it seemed that everyone wanted to get close to him. There was something about connection with the faith leader that brought a sense of comfort and familiarity. There has always been an intersection of faith & freedom. It was faith that sustained our African ancestors through slavery. Whether it’s in terms of freedom from physical bondage, spiritual bondage, or mental bondage, faith has been viewed as the key to unlock the shackles. Within the African American community, there was often a belief that no matter how great the burden, prayer was the answer.
The African American church has traditionally been the gateway into the African American community. It has been our access to social services, family counseling, and a sense of belonging. African American faith leaders also play a pivotal role in community messaging about what is important to black & brown people. We have historically looked to our faith leaders for political guidance, and to be the spokesperson when our communities have needed a champion. As stigma is a significant barrier to accessing the needed support and care for individuals facing mental health concerns, the ability for individuals in distress to have a conversation with a trusted faith leader with whom they have a shared history is often an essential component. It is imperative that our faith leaders are equipped to respond appropriately to the lack of mental health resources in our communities while removing barriers to care.
Our faith leaders can play a pivotal role, if we are to move the needle on improving mental wellness in the African American community. My use of the term “wellness” is intentional; a crucial first step in changing the narrative is to change the language. We should focus on wellness rather than “illness.” Illness implies that something is wrong. Wellness lends itself more easily to viewing treatment as preventive.
If we want to strengthen the role of the church in promoting metal wellness, we must:
- Educate church leaders about mental health, make sure they understand that mental health conditions are just as real (and common) as physical health conditions, and that it is likely that several families in church congregations may be experiencing mental health challenges
- Seek opportunities to collaborate and work together with community mental health providers – imagine how much more comfortable a church member would be accessing his mental health clinician virtually from his local church, rather than visiting a clinician’s office
- Opportunity exists for African American churches and mosques to provide depression education and treatment on their campuses – reach out to community stakeholders and invite them to speak to your congregations about mental health, and include mental health when scheduling health fairs
- Encourage churches and mosques to offer Mental Health First Aid Training at their facility
- Prepare church leaders to recognize mental health symptoms, learn how to have an appropriate conversation about it, and refer congregants to mental health professionals rather than trying to “counsel” them themselves
- Recruit trained mental health professionals to church staff
- Find ways to normalize the conversation and increase social support for those experiencing mental health symptoms.
The topic of mental health is still often associated with a sense of shame among African Americans, making it hard for those experiencing distress to reach out for help, and for those who care about them to help connect them to that help. By spreading awareness and understanding about suicide prevention and mental health, the church can become an important place of refuge for those struggling.
[1] Any Mental Illness (AMI) Among Adults. (n.d.). Retrieved May 1, 2019, from https://www.nimh.nih.gov/health/statistics/mental-illness.shtml#part_154785
[2] Substance Abuse and Mental Health Services Administration, Racial/Ethnic Differences in Mental Health Service Use among Adults. HHS Publication No. SMA-15-4906. Rockville, MD: Substance Abuse and Mental Health Services Administration, 2015. Retrieved July 2017, from https://www.samhsa.gov/data/sites/default/files/MHServicesUseAmongAdults
[3] Religious Coping Among African Americans, Caribbean Blacks and Non-Hispanic Whites.[J Community Psychol. 2008] Chatters LM, Taylor RJ, Jackson JS, Lincoln KD J Community Psychol. 2008 Apr; 36(3):371-386
Preventing Heart Attacks and Strokes
by /www.cdc.gov/vitalsigns/million-hearts/ | February 5, 2022
Preventing 1 Million Heart Attacks and Strokes
Overview
Heart attacks and strokes can be catastrophic, life-changing events that are all too common. Heart disease and strokes are preventable, yet they remain the leading causes of death, disability, and healthcare spending in the US. Alarmingly, many of these events happen to adults ages 35-64—over 800,000 in 2016. Million Hearts® is a national initiative with a network of partners focused on preventing one million heart attacks, strokes, and other cardiovascular events by 2022. Coordinated actions by public health and healthcare professionals, communities, and healthcare systems can and will keep people healthy, optimize care, and improve outcomes within priority populations.
Healthcare professionals and systems can:
- Focus on the ABCS of heart health: Aspirin use when appropriate, Blood pressure control, Cholesterol management, and Smoking cessation.
- Take a team approach—use technology, standard processes, and the skills of everyone in the healthcare system to find and treat those at risk for heart disease and stroke.
- Make sure people who have had a heart attack or stroke get the care they need to recover well and reduce their risk of another event.
- Promote physical activity and healthy eating among their patients and employees.
* Deaths, hospitalizations, and emergency room visits due to heart attack, stroke, and other cardiovascular conditions like heart failure that could be prevented if Million Hearts 2022 actions are taken.
Problem
Heart attacks and strokes are common and preventable.
- More than 1,000 Americans died each day in 2016 from heart attack, stroke, and other events Million Hearts® is trying to prevent.
- Many opportunities to find and treat risk factors are missed every day.
People not taking aspirin as recommended.
People with uncontrolled blood pressure.

Adults not using statins (cholesterol-lowering medicines) when indicated.
Adult smokers.

Adults who are physically inactive.
Populations more at risk.
- Americans aged 35-64 are less likely to use aspirin or statins (cholesterol-lowering medicines) when indicated, and only about half have their blood pressure under control.
- Blacks/African Americans are more likely than whites to develop high blood pressure—especially at earlier ages—and are less likely to have it under control.
- People with mental health and/or substance use disorders use tobacco more frequently.
- People who have already had one heart attack or stroke are at high risk for a second.
Source: Million Hearts® At-A-Glance, 2017
35-64 year olds

In 2016, about 775,000 hospitalizations and 75,000 deaths occurred in younger Americans, who are America’s workforce, parents, partners, and caregivers.
Getting to One Million
Everyone can take small steps to improve their own health, the health of their families and loved ones, patients, communities, and the heart health of our nation. We have to act now.
View large image and text description
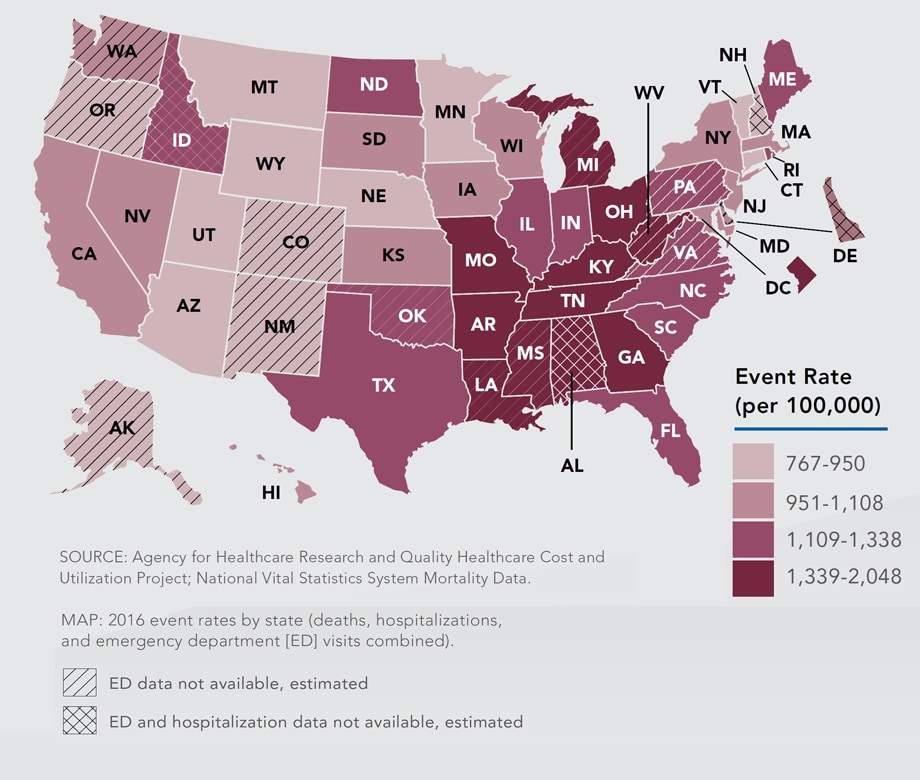
Small changes in every state will have a big impact.
One million events could be prevented by 2022 if every state reduced these life-changing events by 6%.
While rates are higher in the Southeast and Midwest, small changes to improve heart health are needed in all states.
Million Hearts®: Everyone Can Make Small Changes that Matter.
The solution to this crisis is already in front of us. Small changes sustained over time will result in big improvements to the heart health of our nation. Everyone can take action.
Million Hearts® is working with more than 120 partners, all 50 states and the District of Columbia, and 20 federal agencies to:
Keep people healthy by making changes to environments in which people live, learn, work, and play to make it easier to make healthy choices.

HOW: Achieve a 20% reduction in sodium intake, tobacco use, and physical inactivity.

Communities making physical activity easier by creating walking and biking trails.

People adding 10 minutes of physical activity a day—like walking or gardening.
Optimize care so that those at risk for cardiovascular disease get services and skills needed to reduce the risk of having a heart attack or stroke.
- HOW: Achieve 80% performance in the ABCS, and 70% participation in cardiac rehabilitation.
- Insurers providing coverage for home blood pressure monitors.
- Clinicians using a standard treatment protocol for high blood pressure, cholesterol management, and tobacco cessation.
Improve outcomes for priority populations who suffer more from cardiovascular disease and where we know we can make an impact.
- HOW: Employers providing places and time for employees to walk during the workday.
- Behavioral health providers receiving training in smoking cessation and using it in their practice.

Top of Page
We’ve already begun.
Keeping People Healthy.
- Eskenazi Health in Indiana lowered sodium content of foods in all vending machines and cafeterias by 37% with their Choose Health Initiative.
Optimizing Care.
- Over 200 Federally Qualified Health Centers achieved more than 70% performance of the ABCS in 2016 earning a Million Hearts® badge.
Improving Outcomes for Priority Populations—People who have had a heart attack or stroke.
- Dartmouth-Hitchcock Medical Center in New Hampshire achieved 80% cardiac rehab enrollment through liaisons who identified eligible patients and connected them to programs.
What Can Be Done
The Federal Government is:
- Co-leading the Million Hearts® initiative (CDC and the Centers for Medicare & Medicaid Services) to prevent 1 million heart attacks and strokes by 2022. millionhearts.hhs.govExternal
- Helping improve the heart health of millions of Americans by investing in improving delivery of care, including rewarding clinicians for providing care we know works.
- Providing funding and support to all 50 states, the District of Columbia, municipalities, and tribal communities to ensure clinical and public health agencies are working together to prevent heart disease and stroke.
Healthcare Professionals & Systems Can:
- Focus on the ABCS of heart health: Aspirin use when appropriate, Blood pressure control, Cholesterol management, and Smoking cessation.
- Take a team approach—use technology, standard processes, and the skills of everyone in the healthcare system to find and treat those at risk for heart disease and stroke.
- Make sure people who have had a heart attack or stroke get the care they need to recover well and reduce their risk of another event.
- Promote physical activity and healthy eating among their patients and employees.
State And Local Health Departments Can:
- Use their state’s heart disease and stroke events data to drive Million Hearts® actions locally.
- Promote tobacco control interventions, smoke-free environments, and programs to help tobacco users quit.
- Work to improve heart-healthy nutrition and physical activity by promoting the use of healthy food service guidelines and making communities more walkable.
Employers Can:
- Make it easier for employees to get needed medicines, blood pressure monitors, and services by providing insurance coverage with no or low out-of-pocket costs.
- Provide on-site blood pressure monitoring and physical activity programs.
- Ensure smoke-free spaces and access to healthy food and beverages in vending machines and facilities.
Everyone Can:
- Start one heart healthy behavior today – eat a heart-healthy diet, get physically active, or quit smoking! Keep it going to keep your heart healthy now and later in life!
- Learn your heart age and take action to improve it. cdc.gov/heartdisease/heartage.htm
- If you don’t use tobacco, don’t start. If you do, seek help at 1-800-QUIT-NOW or www.smokefree.govExternal.

More information about Million Hearts® and tools you can use are available at millionhearts.hhs.govExternal.
Stories from people who have taken control of their blood pressure are available at https://bit.ly/2N9ahqXExternal.
Top of Page
Issue Details
Related Pages and Resources:
- Vital Signs –Preventing 1 Million Heart Attacks and Strokes [PODCAST – 1:15 minutes]
- Vital Signs –Preventing 1 Million Heart Attacks and Strokes [PSA – 0:60 seconds]
- Vital Signs Issue Details: Vital Signs: Prevalence of Key Cardiovascular Disease Risk Factors for Million Hearts 2022 — United States, 2011–2016, Morbidity and Mortality Weekly Report (MMWR)
- State-Level Variation in Nonfatal and Fatal Cardiovascular Events Targeted for Prevention by Million Hearts 2022, Morbidity and Mortality Weekly Report (MMWR)
- Million Hearts®External
- Million Hearts® Partner OpportunitiesExternal
- CDC’s Division for Heart Disease and Stroke Prevention
- CDC Heart Disease
- CDC Stroke
- Vital Signs: Preventing Stroke Deaths
- Best Practices for CVD Prevention
- Interactive Atlas for Heart Disease and Stroke
- Agency for Healthcare Research and Quality: Cardiovascular Disease PreventionExternal
- About the Healthcare Cost and Utilization ProjectExternal
- Healthcare Cost and Utilization Project PartnersExternal
- Community Strategies for Physical Activity
- Smoking and Tobacco Use
Information for Healthcare Professionals
- Actions GuidesExternal: Hypertension Control, Self-Measured Blood Pressure Monitoring, Tobacco Cessation, Medication Adherence
- ProtocolsExternal: Hypertension Treatment, Tobacco Cessation, Cholesterol Management
- Hypertension Change PackageCdc-pdfExternal
- Cardiac Rehabilitation Change PackageExternal
- Hypertension Control ChampionsExternal
- Million Hearts® for Clinicians: Embed Resources on Your Website
Information for Everyone
- Taking Control of My Blood Pressure: Patient StoriesExternal
- Heart Age Calculator
- Physical Activity for a Healthy Weight
- Tips for Former Smokers®
Other Sites
- MedlinePlus: Heart DiseasesExternal
- MedlinePlus: StrokeExternal
- American Heart AssociationExternal
- American Stroke AssociationExternal
Science Behind the Issue
COVID-19 update; Omicron variant
by References: www.cdc.gov/coronavirus/2019-ncov/variants/omicron-variant.html | January 2, 2022
CDC is working with state and local public health officials to monitor the spread of Omicron. As of December 20, 2021, Omicron has been detected in most states and territories and is rapidly increasing the proportion of COVID-19 cases it is causing.
Omicron Data and Potential Spread
CDC is expecting a surge of COVID-19 cases in the coming days to weeks. Learn more about Omicron variant surveillance and potential rapid spread.
COVID Data TrackerOmicron Potential Spread
What We Know about Omicron
CDC has been collaborating with global public health and industry partners to learn about Omicron, as we continue to monitor its course. We don’t yet know how easily it spreads, the severity of illness it causes, or how well available vaccines and medications work against it.
Spread
The Omicron variant likely will spread more easily than the original SARS-CoV-2 virus and how easily Omicron spreads compared to Delta remains unknown. CDC expects that anyone with Omicron infection can spread the virus to others, even if they are vaccinated or don’t have symptoms.
Severe Illness
More data are needed to know if Omicron infections, and especially reinfections and breakthrough infections in people who are fully vaccinated, cause more severe illness or death than infection with other variants.
Vaccines
Current vaccines are expected to protect against severe illness, hospitalizations, and deaths due to infection with the Omicron variant. However, breakthrough infections in people who are fully vaccinated are likely to occur. With other variants, like Delta, vaccines have remained effective at preventing severe illness, hospitalizations, and death. The recent emergence of Omicron further emphasizes the importance of vaccination and boosters.
Treatments
Scientists are working to determine how well existing treatments for COVID-19 work. Based on the changed genetic make-up of Omicron, some treatments are likely to remain effective while others may be less effective.
We have the Tools to Fight Omicron
Vaccines
Vaccines remain the best public health measure to protect people from COVID-19, slow transmission, and reduce the likelihood of new variants emerging.
- COVID-19 vaccines are highly effective at preventing severe illness, hospitalizations, and death.
- Scientists are currently investigating Omicron, including how protected fully vaccinated people will be against infection, hospitalization, and death.
- CDC recommends that everyone 5 years and older protect themselves from COVID-19 by getting fully vaccinated.
- CDC recommends that everyone ages 18 years and older should get a booster shot at least two months after their initial J&J/Janssen vaccine or six months after completing their primary COVID-19 vaccination series of Pfizer-BioNTech or Moderna.
Masks offer protection against all variants.
- CDC continues to recommend wearing a mask in public indoor settings in areas of substantial or high community transmission, regardless of vaccination status.
- CDC provides advice about masks for people who want to learn more about what type of mask is right for them depending on their circumstances.
Tests can tell you if you are currently infected with COVID-19.
- Two types of tests are used to test for current infection: nucleic acid amplification tests (NAATs) and antigen tests. NAAT and antigen tests can only tell you if you have a current infection.
- Individuals can use the COVID-19 Viral Testing Tool to help determine what kind of test to seek.
- Additional tests would be needed to determine if your infection was caused by Omicron.
- Visit your state, tribal, local, or territorial health department’s website to look for the latest local information on testing.
- Self-tests can be used at home or anywhere, are easy to use, and produce rapid results.
- If your self-test has a positive result, stay home or isolate for 10 days, wear a mask if you have contact with others, and call your healthcare provider.
- If you have any questions about your self-test result, call your healthcare provider or public health department.
What CDC is Doing to Learn about Omicron
CDC scientists are working with partners to gather data and virus samples that can be studied to answer important questions about the Omicron variant. Scientific experiments have already started. CDC will provide updates as soon as possible.
References: www.cdc.gov/coronavirus/2019-ncov/variants/omicron-variant.html
June is Men's Health Month
by https://www.minorityhealth.hhs.gov/mens-health/ | June 3, 2021
Men's Health Month
Stroke Awareness
May 1, 2021
For African Americans, stroke is more common and more deadly - even in young and middle-aged adults - than for any ethnic or other racial group in the United States.
Learning about stroke can help you act in time to save a co-worker, friend, or relative. And making changes in your lifestyle can help you prevent stroke.
New treatments are available that greatly reduce the damage caused by a stroke. But you need to arrive at the hospital within 60 minutes after symptoms start to prevent disability. Knowing stroke symptomsn (view health tips page), calling 911 immediately, and getting to a hospital are critical.
What is a Stroke?
A stroke is serious - just like a heart attack. A stroke is sometimes called a "brain attack." Most often, stroke occurs when blood flow to the brain stops because it is blocked by a clot. The brain cells in the immediate area begin to die because they stop getting the oxygen and nutrients they need to function.
What Causes a Stroke?
There are two kinds of stroke. The most common kind of stroke, called ischemic stroke, is caused by a blood clot that blocks or plugs a blood vessel in the brain. The other kind of stroke, called hemorrhagic stroke, is caused by a blood vessel that breaks and bleeds into the brain.
What Disabilities can result from a stroke?
Stroke damage in the brain can affect the entire body - resulting in mild to severe disabilities. These include paralysis, problems with thinking, problems with speaking, and emotional problems.
Stroke Symptoms
Sudden numbness or weakness of the face, arm, or leg (especially on one side of the body)
- Sudden confusion, trouble speaking or understanding speech
- Sudden trouble seeing in one or both eyes
- Sudden trouble walking, dizziness, loss of balance or coordination
- Sudden severe headache with no known cause
Because stroke injures the brain, you may not realize that you are having a stroke. The people around you might not know it either. Your family, friends, or neighbors may think you are confused. You may not be able to call 911 on your own. That's why everyone should know the signs of stroke - and know how to act fast.
Don't wait for the symptoms to improve or worsen. If you believe you are having a stroke - or someone you know is having a stroke - call 911 immediately. Making the decision to call for medical help can make the difference in avoiding a lifelong disability.
Call 911
If you believe you are having a stroke - or someone you know is having a stroke - call 911 immediately.
Know Stroke Prevention
Conditions that can cause stroke are very common among African Americans. The best treatment for stroke is prevention. You can reduce your risk of having a stroke by taking action to improve your health.
- Manage your diabetes
- Eat right
- Control your high blood pressure
- Exercise
- Don't smoke
- If you have high blood pressure, work with your doctor to get it under control. Many people do not realize they have high blood pressure, which usually produces no symptoms but is a major risk factor for heart disease and stroke. Managing your high blood pressure is the most important thing you can do to avoid stroke.
- If you smoke, quit.
- If you have diabetes, learn how to manage it. As with high blood pressure, diabetes usually causes no symptoms but it increases the chance of stroke.
- If you are overweight, start maintaining a healthy diet and exercising regularly.
Where Can You Learn More About Stroke?
Talk to your doctor about your personal risk factors for having a stroke. For more information about stroke prevention and treatment, call the National Institute of Neurological Disorders and Stroke at 1-800-352-9424.
Reference: https://www.stroke.nih.gov/materials/needtoknow.htm
Heart Disease: It Can Happen at Any Age
by National Center for Chronic Disease Prevention and Health Promotion , Division | February 1, 2021
Heart Disease: It Can Happen at Any Age
Heart disease doesn’t happen just to older adults. It is happening to younger adults more and more often. This is partly because the conditions that lead to heart disease are happening at younger ages.
February is American Heart Month, the perfect time to learn about your risk for heart disease and the steps you need to take now to help your heart.
Heart disease—and the conditions that lead to it—can happen at any age.
High rates of obesity and high blood pressure among younger people (ages 35–64) are putting them at risk for heart disease earlier in life.
Nearly half of all Americans have at least one of the top three risk factors for heart disease: high blood pressure, high cholesterol, and smoking.1,2

Learn about your risk for heart disease and the steps you need to take now to help your heart.
You Could Be at Risk
Many of the conditions and behaviors that put people at risk for heart disease are appearing at younger ages:
- High blood pressure. Millions of Americans of all ages have high blood pressure, including millions of people in their 40s and 50s. About half of people with high blood pressure don’t have it under control. Having uncontrolled high blood pressure is one of the biggest risks for heart disease and other harmful conditions, such as stroke.
- High cholesterol. High cholesterol can increase the risk for heart disease. Having diabetes and/or obesity, smoking, eating unhealthy foods, and not getting enough physical activity can all contribute to unhealthy cholesterol levels.
- Smoking. More than 35 million U.S. adults are current smokers, and thousands of young people start smoking each day.3,4 Smoking damages the blood vessels and can cause heart disease.
On average, U.S. adults have hearts that are 7 years older than they should be. Watch this video to learn about “heart age.”
Other conditions and behaviors that affect your risk for heart disease include:
- Obesity. Carrying extra weight puts stress on the heart. More than 1 in 3 Americans—and nearly 1 in 6 children and adolescents ages 2 to 19—have obesity.5
- Diabetes causes sugar to build up in the blood. This can damage blood vessels and nerves that help control the heart muscle. More than 1 in 10 people in the United States have diabetes.6
- Physical inactivity. Staying physically active helps keep the heart and blood vessels healthy. Only 1 in 4 adults meet the physical activity guidelines of getting 150 minutes of moderate-intensity activity per week.7
- Unhealthy eating patterns. Most Americans, including children, eat too much sodium (salt), which increases blood pressure.8 Replacing foods high in sodium with fresh fruits and vegetables can help lower blood pressure. Only about 1 in 10 adults get enough fruits and vegetables each day.9,10 A diet high in trans fat, saturated fat, and added sugar increases the risk factor for heart disease.
4 Ways to Take Control of Your Heart Health
You’re in the driver’s seat when it comes to your heart. Learn how to be heart-healthy at any age.
Don’t smoke. Smoking is the leading cause of preventable death in the United States. If you don’t smoke, don’t start. If you do smoke, learn how to quit.
Manage conditions. Work with your health care team to manage conditions such as high blood pressure and high cholesterol. This includes taking any medicines you have been prescribed. Learn more about preventing and managing high blood pressure and high cholesterol.
Make heart-healthy eating changes. Eat food low in trans fat, saturated fat, added sugar, and sodium. Try to fill at least half your plate with vegetables and fruits, and aim for low sodium options. Learn more about how to reduce sodium.
Stay active. Get moving for at least 150 minutes per week.11 You can even break up the exercise into 10-minute blocks for a total of 30 minutes in a day. Learn more about how to get enough physical activity.
More Information
CDC
National Heart, Lung, and Blood Institute
American Heart Association
Page last reviewed: January 26, 2021
Content source: National Center for Chronic Disease Prevention and Health Promotion , Division for Heart Disease and Stroke
COVID-19 Vaccination Program
by National Center for Immunization and Respiratory Diseases (NCIRD), Division of V | December 31, 2020
Updated Dec. 22, 2020
Now that there are authorized and recommended vaccines to prevent COVID-19 in the United States, here are 8 things you need to know about the new COVID-19 Vaccination Program and COVID-19 vaccines:
The safety of COVID-19 vaccines is a top priority.
The U.S. vaccine safety system ensures that all vaccines are as safe as possible. Learn how federal partners are working together to ensure the safety of COVID-19 vaccines. The CDC has developed a new tool, v-safe, as an additional layer of safety monitoring to increase our ability to rapidly detect any safety issues with COVID-19 vaccines. V-safe is a new smartphone-based, after-vaccination health checker for people who receive COVID-19 vaccines.
COVID-19 vaccination will help protect you from getting COVID-19. Two doses are needed.
Depending on the specific vaccine you get, a second shot 3-4 weeks after your first shot is needed to get the most protection the vaccine has to offer against this serious disease. Learn more about the benefits of getting vaccinated.
CDC is making recommendations for who should be offered COVID-19 vaccine first when supplies are limited.
To help guide decisions about how to distribute limited initial supplies of COVID-19 vaccine, CDC and the Advisory Committee on Immunization Practices have published recommendations for which groups should be vaccinated first.
Learn more about who should be vaccinated first when vaccine supplies are limited.
There is currently a limited supply of COVID-19 vaccine in the United States, but supply will increase in the weeks and months to come.
The goal is for everyone to be able to easily get vaccinated against COVID-19 as soon as large enough quantities are available. Once vaccine is widely available, the plan is to have several thousand vaccination providers offering COVID-19 vaccines in doctors’ offices, retail pharmacies, hospitals, and federally qualified health centers.
After COVID-19 vaccination, you may have some side effects. This is a normal sign that your body is building protection.
The side effects from COVID-19 vaccination may feel like flu and might even affect your ability to do daily activities, but they should go away in a few days. Learn more about what side effects to expect and get helpful tips on how to reduce pain and discomfort after your vaccination.
Making COVID-19 Vaccination Recommendations
CDC makes vaccination recommendations, including those for COVID-19 vaccines, based on input from the Advisory Committee on Immunization Practices. Learn more
Cost is not an obstacle to getting vaccinated against COVID-19.
Vaccine doses purchased with U.S. taxpayer dollars will be given to the American people at no cost. However, vaccination providers may be able to charge administration fees for giving the shot. Vaccination providers can get this fee reimbursed by the patient’s public or private insurance company or, for uninsured patients, by the Health Resources and Services Administration’s Provider Relief Fundexternal icon.
The first COVID-19 vaccine is being used under an Emergency Use Authorization (EUA) from the U.S. Food and Drug Administration (FDA). Many other vaccines are still being developed and tested.
Learn more about FDA’s Emergency Use Authorization authorityexternal icon and watch a video on what an EUA is.
If more COVID-19 vaccines are authorized or approved by FDA, the Advisory Committee on Immunization Practices (ACIP) will quickly hold public meetings to review all available data about each vaccine and make recommendations for their use in the United States. Learn more about how CDC is making COVID-19 vaccine recommendations.
All ACIP-recommended vaccines will be included in the U.S. COVID-19 Vaccination Program. CDC continues to work at all levels with partners, including healthcare associations, on a flexible COVID-19 vaccination program that can accommodate different vaccines and adapt to different scenarios. State, tribal, local, and territorial health departments have developed distribution plans to make sure all recommended vaccines are available to their communities.
COVID-19 vaccines are one of many important tools to help us stop this pandemic.
It’s important for everyone to continue using all the tools available to help stop this pandemic as we learn more about how COVID-19 vaccines work in real-world conditions. Cover your mouth and nose with a mask when around others, stay at least 6 feet away from others, avoid crowds, and wash your hands often.
CDC will continue to update this website as vaccine recommendations and supply change.
Last Updated Dec. 22, 2020
Content source: National Center for Immunization and Respiratory Diseases (NCIRD), Division of Viral Diseases
Holiday Depression and Stress
by WebMD Medical Reference | December 3, 2020
The holiday season for most people is a fun time of the year filled with parties, celebrations, and social gatherings with family and friends. For many people, it is a time filled with sadness, self-reflection, loneliness, and anxiety.
What causes holiday blues?
Sadness is a truly personal feeling. What makes one person feel sad may not affect another person. Typical sources of holiday sadness include:
- Stress
- Social isolation
- Loss of a loved one - this feeling may happen during the holiday season for years after the loss
- Over-commercialization
- Financial stress
- The inability to be with one's family and friends due to COVID-19
19 tips for coping with holiday stress and depression:
- Pray for the stronghold of depression to be lifted. Let your inner "joy" help you to remember the blessings of life and tomorrow's promise!
- Make realistic expectations for the holiday season.
- Cherish the memories you had with loved ones who have passed away, knowing that they are always with you in spirit.
- Pace yourself. Do not take on more responsibilities than you can handle.
- Make a list and prioritize the important activities. This can help make holiday tasks more manageable.
- Be realistic about what you can and cannot do.
- Make time for yourself! Try to take at least 30 minutes - 1 hour a day of quiet time to meditate and decompress.
- Do not put all your energy into just one day (i.e., Thanksgiving Day, New Year's Eve). The holiday cheer can be spread from one holiday event to the next.
- Live and enjoy the present.
- Look to the future with optimism.
- Don't set yourself up for disappointment and sadness by comparing today with the good old days of the past.
- Find holiday activities that are free, such as looking at holiday decorations, going window shopping without buying, and watching the winter weather, whether it's a snowflake or a raindrop.
- Limit your drinking, since excessive drinking will only increase your feelings of depression.
- Try something new. Celebrate the holidays in a new way.
- Spend time with supportive and caring people.
- Reach out and make new friends.
- Make time to contact a long-lost friend or relative and spread some holiday cheer.
- Donate time or money to organizations that serve holiday meals to those in need.
- Keep track of your holiday spending. Overspending can lead to depression when the bills arrive after the holidays are over. Extra bills with little budget to pay them can lead to further stress and depression.
- People change behaviors when there is less sunlight. Most people find they eat and sleep slightly more in wintertime and dislike the dark mornings and short days. For some, however, symptoms are severe enough to disrupt their lives and to cause considerable distress. These people may be suffering from seasonal affective disorder (SAD).
- Research studies have that found phototherapy is effective in treating people that suffer from SAD. Phototherapy is a treatment involving about a half hour a day of exposure to artificial sunlight. For many sufferers of SAD, phototherapy can be a highly effective treatment either alone or in combination with medicines, psychotherapy, or both."
© 2020 WebMD, LLC. All rights reserved.
| << Previous 1 - 2 Next >> |